Chronic headache
I’m very brave generally,” he went on in a low voice: “only today I happen to have a headache.
-Lewis Carroll
The impact of chronic headache
Headache is a major health issue. There are many different types of headache with tension-type headaches, migraine headaches and medication overuse headaches (MOH) being the most common. Just migraine alone affects 12-15% of our population and is the second leading cause of disability globally (after lower back pain), and is the most common cause of disability in young women. Migraines are three times most common in women (occurring in up to 17% of women) than men (occurring in up 6% of men). Migraine is most common in those 20-50 years old with a peak incidence in peoples’ 30s. When a headache happens more days than not, it is called chronic. Chronic headache affects about 4% of the world’s adult population, again, most commonly young women (20-50 years old).
The symptoms of headache
Most people think that a headache comes in when your head starts to hurt. However, headaches actually begin several hours before your head starts to hurt and end several hours after your head stops hurting. For example, the image below summarizes this for migraines.
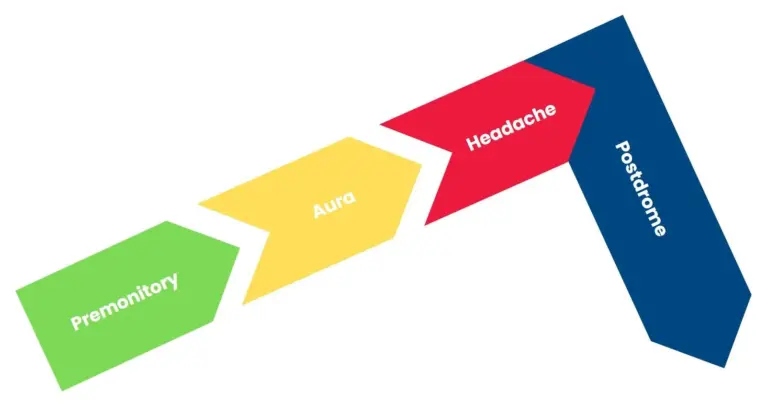
You can think of the headache as the storm and the premonitory phase as the quiet before the storm, and the postdrome phase as the quiet after the storm. Many symptoms occur during these pre- and post- headache times such as:
- drowsiness
- irritability
- difficulty with concentration
- yawning, nausea
- stiff neck/neck pain
- changes in appetite
- sensory hypersensitivities (i.e., like being sensitive to light, sound, smell, etc.)
- food cravings
- changes in mood for better or for worse
- and more.
During the headache phase, people can experience many symptoms depending on their diagnosis. For example, migraine patients can experience many neurological symptoms like visual disturbances, weakness and dizziness. In fact, the leading cause of dizziness is migraine.
And then many people with chronic headaches also have other health issues. Going back to the example of migraine, there is a high incidence of many health issues in those with chronic migraine such as:
- Depression
- Anxiety
- Panic disorder
- Chronic fatigue syndrome
- Insomnia
- Fibromyalgia
When treating patients it becomes important to treat the patient (i.e., address all of this) rather than just treat the headache.
The neuropsychological underpinnings of headache (i.e., What is a headache?)
Headache is an experience. And an experience is most fundamentally explained by showing you the way that your brain lights up while your experiencing something. For headaches, a network of brain structures known as the pain matrix lights up. This experience is your reality; it’s the way you feel the headache. It’s more reliable and accurate than a diagnostic checklist or a biochemical (i.e., mechanism of chemicals and receptors) explanation of headache. The parts of the brain that sit on this pain matrix are the parts that process many aspects of the pain experience:
Sensory-discriminative
- i.e., Primary Sensory Cortex, Posterior Insula
- Processes signals coming from nerve endings in your body
- This is what many erroneously refer to as “physical pain”…But to only consider this part of the pain experience would be analogous to only acknowledging one instrument in a symphony.
Affective Motivational
- i.e., Anterior Cingulate Cortex, Anterior Insula, Amygdala
- Processes the feeling of being in pain, fear of pain, wanting to avoid pain, etc.
Cognitive
- i.e., Prefrontal Cortex, Hippocampus
- Processes how much attention you pay to pain, expectations of your condition, past memories of this pain, etc.
Integrative
- i.e., Middle Cingulate, Temporal Cortex, Pulvinar
- Coordinates and processes communication between parts of this pain matrix
- This is kind of like muscle memory, except, nobody wants to get good at having headaches.
This is why treatments that work on cognitive circuits and emotional circuits in the brain work! They are just as evidence-based as medication, and even more effective in the long-run; i.e., medication tend to only work for as long as you take them. So, what are the right treatments for any given person? Since all people are unique, the way people use these regions of the brain in day-to-day life is also unique. Hence, treatments must be custom-tailored to the patient. And since nobody knows the patient as well as the patient themselves, they must participate in discovering the treatment plan. In this context, doctors generally just prescribe medication and guide the patient through a process of discovery just as a coach would help an athlete discover the best way they can perform their sport. This is what is known as the functional model of headache management. It draws on many different types of treatment as discussed in our page on the headache management.
Headache treatments
Most of the focus of headache treatment – if not all in many patients – is on medication. However, other treatments have been shown to be just as effective in most patients, and even more effective in the long run. Certain medications have evidence in certain conditions. Interestingly, most prophylactic medications for migraine were originally intended for other conditions:
- antidepressants
- anti-hypertensives
- anti-convulsants
- anti-inflammatories, etc.
There are also injectable medications like local anesthetic and onabotulinumtoxin A that have been discovered to be helpful for migraines. There are also the new class of CGRP medication which have been developed to target and interrupt the migraine biochemical pathway. However, the neurophysiological evidence that the mechanisms between different types headaches are really different is a bit limited. In other words, there is no evidence that our brains experience different types of headaches differently. Also, the evidence that different types of headache respond differently to behavioral treatment is limited. Moreover, for certain types of headaches – like Post-traumatic headache (PTH) – there is no evidence that medication are even useful.
Non-medication treatments are very powerful and shouldn’t be seen as competing with medication. For example, in those migraine patient who have insomnia, correcting their sleep through CBT-i can improve their headaches by 60%, which is a more robust an improvement than medications in general. Both classes of treatment (medicinal and non-medicinal) are on the same side: there to make you feel better. In fact, behavioural & lifestyle interventions improve how effectively medication work. You can read more about behavioural & lifestyle interventions for headache in our page headache management.
What happens to headache if you do nothing about it and try to wait it out?
The data on this depends on the type of headache you have but in chronic migraine headache for example, 26 to 70% of patients will move from having headaches more often than not to having headaches on more days of the month than headache days. Many of these patients who see improvement also have been seen to use medication less, use necessary medication regularly and skillfully and stick to lifestyle regimens like regular physical exercise.
Who is a Good Candidate for Managing Their Headaches Functionally?
This is best suited for those with chronic headache (have headaches more often than not) who are willing to do what it takes to improve their lives. This is also a good option for those taking medication as it will generally improve their treatment further. This is an especially good option for those who can’t take medication or prefer not to.
Proposed OHIP-Funded Group Counselling Training Sequence

Headache Behavioural Therapy
Leveraging your behaviours to see headaches fall by the wayside
Headache management offered in...

Medical Assessment
OHIP-funded medical assessments for behavioural & lifestyle interventions